
A Guide on Interpreting the Outcome
Let’s again assume that you’ve antibodies against the latest Coronavirus. Now, would that suggest that you won’t get sick again? The reinfection Problem is “a mystery. We don’t know because the virus is still brand fresh.
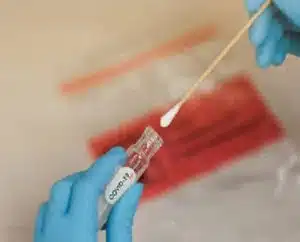
Antibody kits: A relevant case. Some patients from China, South Korea, and Japan left the hospital after having screened negative for the disease and were subsequently readmitted. Even more, these people again came out positive for the illness. We don’t know exactly yet, but typically, certain viruses can’t re-infect people for months or years. The samples used on the PCR test likely gave false negatives.
It is also possible for people to start excreting viral fragments that occur after the disease has passed in research. The rectal swabs and stool culture stay healthy for around a month, which has little to do with the transmission. There are all pieces of digested infection. There are some positive indicators of defence being provided by pathogens. One represents the serum treatment. Here, the doctors spin off portions of the blood that contain pathogens from Covid-19 patients. They then give it to ill persons.
In a sample of 10 patients, the conditions of those people being provided with the survivors’ serum “significantly enhanced.” The research is too limited to be conclusive. However, it does indicate that it may be a smart strategy for more prominent serum antibody test kits.
Does the number of kits matter?
We don’t know once again. Experts’ opinions on results from COVID-19 test kits differ by far. After all, it’s too early to say what might act as defensive signs. It is still too early to tell to what degree an individual who recovered from the disease might be a suitable serum donor. The overall sum of viruses in patients’ blood ranges greatly. Younger individuals using medical options often have fewer risks. Young people who screen positive for the STI virus and survive have almost no neutralizing antibodies.
Some patients using a PCR test displayed weak sample rates. This likely is when specific segments of the immune system target the virus and kill it. Yet the pathogens and the cells that produce them are the keys to maintaining themselves safe. Here, too, the low rates of pathogens will make it challenging to analyze population-level data.
Can we get appropriate STI Lab Test Kit cases if anyone has been contaminated but hasn’t developed antibodies? Will the current solutions help in this? For other Coronaviruses— some that induce the common cold — how people produce these tend to differ by age. Further, people over the age of 60 are more reliable at producing those that neutralize the virus as well as those that warn killer cells of the immune system.
Final Thoughts on Exams
Medical options might be helpful in another way, but it’s pretty far out. We realize that for PCR Tests and COVID, most vaccinations function by developing an antibody response.
